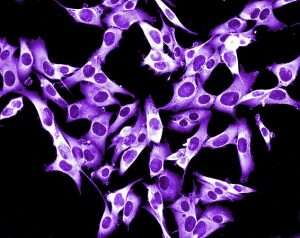
Tel Aviv University researchers reported a breakthrough in melanoma treatments this week, saying they have developed a nanotechnology system that will increase the effectiveness of treating melanoma skin cancer and its metastases by better-transporting drugs to the cell area.
The team is lead by Professor Ronit Satchi-Fainaro, head of the Department of Physiology and Pharmacology at TAU's Sackler School of Medicine.
Follow Israel Hayom on Facebook and Twitter
According to Satchi-Fainaro, the treatment is designed to address the resistance some cancer cells develop to drugs over time.
The drug-carrying system seeks to enable doctors to use two or more treatments to attack cancer cells from different directions, simultaneously, and with greater intensity. This way, it will be possible to delay and even prevent the development of drug resistance.
"The study seeks to solve a common problem related to drug cocktails," she explained. "Currently, most oncology treatments comprise several drugs that are given to the patient at the same time, but nevertheless do not reach the tumor at the same time as they differ from each other in terms of how long they remain in the bloodstream and the time it takes them to reach a tumor.
"Therefore, in most cases, the drugs don't work in a way that allows for significant synergy."
To address these challenges, the researchers chose two known biological drugs for melanoma and attempted to deliver them to the tumor using a nanometric carrier.
The carrier chosen for the task was a PGA polymer, developed in Satchi-Fainaro's lab, which has previously been successfully tested on animals to treat a variety of treatments for pancreatic, breast, and ovarian cancer.
In the first phase, the researchers examined the optimal ratio between the two melanoma drugs, to maximize synergy according to several criteria: toxicity type and level, and the resistance mechanism that the tumor develops towards each drug.
This determines an optimal ratio, ensuring maximal efficiency and minimal toxicity.
Another significant advantage of combining the drugs with the carrier is using a smaller dose, much lower than the dose each drug would require individually.
Next, researchers matched the PGA carrier with the selected drugs by changing its chemical structure, to optimize the match between them.
This integrated system passes through the body safely, without compromising healthy tissues. When it encounters a cancer cell, the protein breaks down the polymer and releases the drugs, which become active and attack the tumor.
"It's like having several passengers take the same cab to the same place. Everyone arrives at their destination at the same time," Satchi-Fainaro said.
She noted that "the platform we have developed is modular in nature, and it can fit a wide range of drugs. We believe it has tremendous potential for treating a huge variety of diseases."
Subscribe to Israel Hayom's daily newsletter and never miss our top stories!




